Why aren’t effective lifestyle strategies
routinely ‘prescribed ‘to manage Type 2 diabetes?
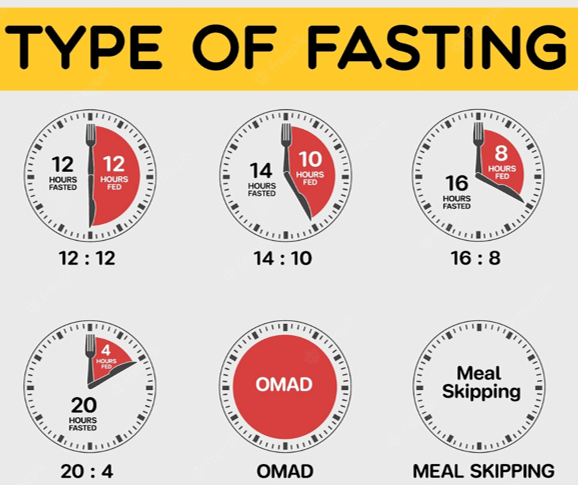
There are simple lifestyle-based approaches that will improve and even remit Type 2 diabetes: Intermittent fasting, minimal processed food and light exercise leading to weight loss all play a part in that – so what is the answer, why not ‘prescribe’ it? What follows are own opinions (based on research natch!) are in the slider below. Let me know what you think in the comments section…





Worryingly, it’s seems that healthcare guidelines used by the NHS and other health institutions often lag behind (nutritional) science somewhere between 10–20 years, so it’s the health system and medical guidelines that are out of date and need changing to match the latest research
10 yrs or more to set new
guidelines
A further 5 yrs or more to train
NHS Staff
This means 15+ yrs to update treatment pathways. Disaster!

#2 : Outdated Training? Just Following NHS Guidelines...
Historically, clinicians receive very little nutrition, lifestyle, or weight-management training in medical/nursing school
This may be changing slowly but speaking generally, critical lifestyle aspects that improve health are lagging behind the research by many years due to the need to update treatment and training guidelines
Patient Behavioural change leading to remission-focused lifestyle programs are almost always absent from the curriculum in any meaningful way
#3: Clinical Guidelines Are Historically Focused On Type 2 Management Not Remission
Until recently (c2017), remission of T2D was considered rare or even impossible.
Guidelines emphasised:
🧩 medication escalation
🧩 preventing complications
🧩 maintaining “acceptable” HbA1c


Management vs Remission
Remission as a goal is still only slowly entering mainstream guidelines

Outdated Practices
Because guidelines shape practice, many clinicians are simply following what they were taught.

Treating Causes Not Symptoms
Current treatments focus on managing symptoms not targeting the root causes

Fixing The Root Causes
Intermittent fasting, minimal processed food, light exercise leading to weight loss all play a part in resolving root causes


Intermittent Fasting (IF) can cause hypoglycaemia (low blood sugar) in some people that are medicated and taking:
💉insulin
💊sulfonylureas (e.g. gliclazide) or
🧂certain other drug combinations (may not be diabetes related drugs)
it’s estimated that for approx. 5-10% of people that are on glucose-lowering medication, recommending fasting without intensive monitoring can be dangerous and continuous monitoring is highly recommended. So very possible then!


In the modern age, appointment times are very limited and budgets are under severe pressure. This means the very things that can lead to remission are overlooked. Typically, medical staff simply don’t have time or resources (including the money!) to manage T2 through to remission, even if guidelines allowed them to do so
Clinicians often avoid suggesting something that requires:
🩺 medication de-prescribing (training)
💰 continuous glucose monitoring (cost)
👀 time consuming supervision (time/cost)

#5: Time constraints do not provide positive outcomes
Diagnosis takes time...
...but time is in short supply
⏱️ Most GP appointments are 7–10 minutes long making meaningful dietary counselling almost impossible
A proper lifestyle conversation requires:
📢 20–40 minutes
📢 personalised advice
📢 Testing and results review
📢 reviewing diet/eating patterns
📢 setting goals
📢 explaining fasting safely
📢 medication adjustments and follow-up




Assumptions about patients are often made:
🙃 People won’t stick to fasting
🙃 People won’t give up processed foods
🙃 People prefer medications to making major changes
As a result, clinicians may default to what they expect the patient to follow but research shows this assumption isn’t always true — many people will follow structured lifestyle programs when properly supported
Clinicians do not want to “promise too much" but this conservative approach may be to the detriment of the patient who can follow this path - if not into remission but certainly to improve type 2 prognosis


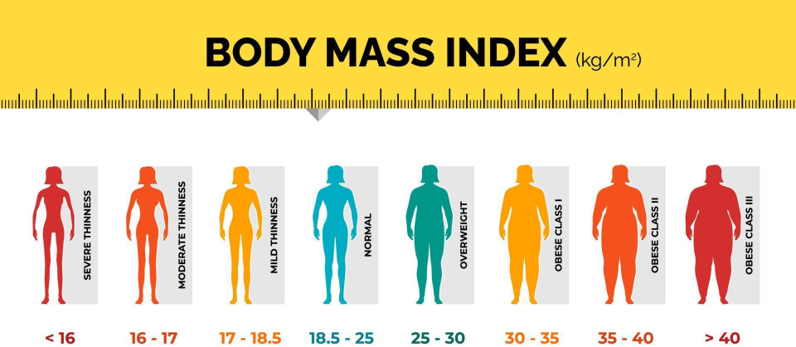
Although fasting and real-food diets help many people, remission likelihood varies by:
🌦️ duration of diabetes | 🌦️ comorbidities
🌦️ weight | 🌦️ visceral fat
🌦️ pancreatic beta-cell reserve | 🌦️medications
Some clinicians avoid strong lifestyle messaging because they don’t want patients to feel:
😌 upset
😌 shamed
😌 blamed
😌 judged
This leads them to soften or avoid strong dietary advice which exacerbates the problem many times over


Patients often receive vague advice (“eat healthier”, “exercise more”) with no practical steps, no personalised approach, and no structured plan
Lifestyle change can feel unmanageable — too many changes at once, too much information, and no phased or simple starting point
Many have tried diets or exercise plans before and “failed”, creating a belief that lifestyle changes don’t work for them
Long gaps between appointments and no ongoing coaching or follow-up make behaviour change harder to sustain
Ultra-processed food is everywhere. Family habits, workplace food, stress and time pressure all push people toward convenience
Medication can help quickly; lifestyle takes weeks or months. Patients may lose momentum before seeing results
Patients are overwhelmed by conflicting messages — low-fat vs low-carb, snacking vs fasting, etc. This creates doubt, paralysis, and mistrust
Stress, anxiety, poor sleep, depression and emotional eating undermine consistency and motivation
low confidence
against you!
down to you and only you

These options are often sold as “wholesome” or “high protein”, but they’re usually full of added sugar and refined carbs, which spike blood glucose and leave you hungry again.
Liquid sugar is one of the fastest ways to raise blood glucose. These drinks add a lot of sugar without making you feel full.
These products look balanced but are usually made from refined flour, sweetened sauces and industrial oils, leading to big glucose spikes.
Even when labelled “wholemeal” or “brown”, these are often highly processed and behave much like white bread inside the body.
Marketed as performance or wellness products, many are just sweets in disguise, full of sugars, starches and additives.
Packaging and claims (“no added sugar”, “wholegrain”) hide the fact that most kids’ products are very sweet and ultra-processed.
Seek Healthy Alternatives!!

The rise in type 2 diabetes and obesity parallels a major increase in ultra-processed food (UPF) consumption. Growing research shows that higher UPF intake raises the risk of both conditions — for each additional 10% of your diet that comes from UPFs, the risk of type 2 diabetes rises by roughly 13%. While causation isn’t fully proven, the consistency of the evidence makes UPFs a credible and modifiable driver of the epidemic
#9: Prepare for change!
With better understanding, smarter strategies, and a little support, lifestyle changes can easily made, yes, I said easily!
📢Begin with one small change and keep going
🤗 our bodies want to heal.
🤗 biology responds quickly.
📢 You are capable of much more than you realise!

📢 Real Change Starts With Better Tools, Better Knowledge, and Better Support - and, of course, with YOU
🔒 Most people don’t struggle because they’re “not disciplined”
🔒Environment, food and healthcare systems make lifestyle change difficult
🔓 With clear guidance, progress is both possible and sustainable
🔑 Let’s change the story.
🔑 Use lifestyle medicine to help take control of your health
👀
📢 Now that you’ve seen the barriers, the next step is simple:
✔ Browse this site, get the simpler guidance
✔ Stop feeling confused
✔ Build your confidence
✔ Commit to change and smash it!!
👉 👥Together we can transform your diabetes care, one practical step at a time
📢 Start making small, meaningful changes today — momentum builds fast
Your Health | Your Responsibility
















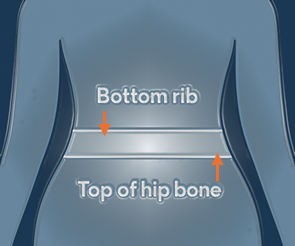
 Use a flexible tape measure (Doh!)
Use a flexible tape measure (Doh!)
 Feel for your bottom rib with your fingers
Feel for your bottom rib with your fingers
 Feel for the top of your hip bone
Feel for the top of your hip bone